Treating Decay Subgingivally with a Soft Tissue Diode Laser
exposed to potential decay. Often when oral hygiene is inadequate, patients have dry mouth or have abfractions, tooth structure can be affected, and the decay process begins. Many patients have recurrent decay around existing Class V restorations, which is a significant issue. To attain a long-term restorative result, it is essential to ensure an adequate marginal seal around all aspects of the cementum-enamel restoration, which requires optimal isolation. A rubber dam can help, but only if the tissue can be retracted effectively.

FIG. 1
is a portable 5W 810nm soft tissue laser. The 810nm wavelength is highly absorbable by hemoglobin and melanin, resulting in minimal bleeding, and allows for
rapid healing of the wound. The Bluewave diode laser is very cost-efficient, lightweight, battery operated, and portable to easily move between operatories. The unit occupies a small footprint of counter-space and the laser handpiece is held securely in place with a magnetic cradle for increased protection against accidental dislodgement and breakage.

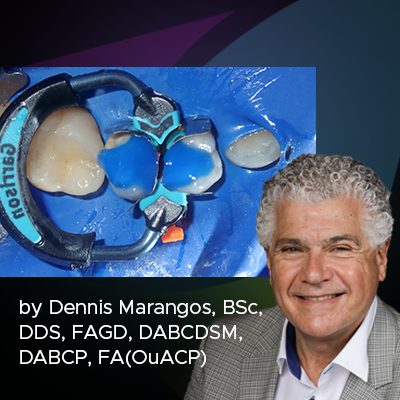
FIG. 2
Initially, the decay was removed up to the free gingival margin. (FIG. 2) The retraction cord would not have retracted the tissue enough to complete the caries
removal, so the laser procedure was utilized. The patient had already been anesthetized; however, additional anesthetic was placed in the buccal area adjacent to
the prepared teeth. Prior to initiating laser treatment, a flexible periodontal probe (Hu-Friedy) was inserted into the periodontal pocket to determine where the
level of the bone was positioned in order to prevent impingement of the biological width. The biologic width was determined to be approximately 2-3mm, indicating
adequate gingival tissue for a soft tissue laser procedure. In preparation for the procedure, the patient and all staff present had laser eye protection placed and a disposable, pre-bent tip was inserted into the Bluewave handpiece.
When using a laser, the laser beam is always directed away from the eyes and should always utilize the minimum power setting necessary to accomplish the procedure. If the laser tip drags while the laser is in active mode and is moving across the tissue, the power is too low. Simply increase the power as needed for the smooth removal of the tissue. On the other hand, if there is excess burning or blackening of the tissue, this is an indicator that the power level is too high. In this case, the Bluewave laser was set at a preset power setting of one (1) watt. (FIG. 3)

FIG. 3
Clinically, the tissue was slightly inflamed due to the presence of decay and bacterial infiltration. This tissue was removed with the Bluewave laser to the level where the decay could be removed, and healthy tooth structure could be adequately isolated and restored. (FIG. 4)

FIG. 4
Following the laser tissue removal, a #0 retraction cord with ferric sulfate was placed to further hold the tissue in place and keep the area moisture-free. Although the tissue was isolated and retracted, there was some minimal bleeding present, which prevented a completely dry field. Retraction paste (3M™) was placed around both tooth preparations and completely covered the recently lasered tissue and cord. (FIG. 5) The retraction paste was allowed to set for 5 minutes. The paste was gently
rinsed off to prevent rebound bleeding and the area was dried.

FIG. 5
After complete decay removal, the deeper areas of the preparation were protected with Vitrebond™ (3M). (FIG. 6) The preparation was then etched with 37% phosphoric acid, rinsed then lightly dried. G5™ desensitizer (Clinician’s Choice) was scrubbed into the preparation to prevent post-op sensitivity, with the excess G5 blotted with a micro brush. A bonding agent was applied, thinned, and then light-cured with the VALO™ Grand (Ultradent™). Flowable composite was heated in the Calset™ Composite Warmer (AdDent) and placed along the cervical aspect of the preparation and light-cured, to establish a gap-free marginal seal. Additional flowable composite was then spread coronally to ensure thorough coverage of the cementum. This was followed by heated microfill composite, placed in
increments and then using a REJ #04(Clinician’s Choice) to completely fill the preparation. Care was taken before to smooth the composite as much as possible and remove excess before light-curing in order to minimize the amount of finishing time required. (FIG. 7)

FIG. 6

FIG. 7
Excess composite was removed, and the restoration was shaped using a thin tapered diamond bur. Coarse and medium grit Contours™ Finishing and Polishing Discs (Clinician’s Choice) were used to smooth and refine the restoration. Finally, the A.S.A.P® 2-step diamond polishing system (Clinician’s Choice) quickly created a high-luster polish, essential for preventing stain and plaque formation and contributing to the longevity of the restoration.
The one-week follow up photo shows how well the tissue healed after utilizing the Bluewave laser. (FIG. 8) The use of a soft tissue laser in dentistry benefits the patient over traditional surgical procedures in a less traumatic procedure and a shortened recovery time with minimal post-op discomfort. The dentist benefits because the restoration can be completed in the same day, is very easy to use with proper training, and is very cost-effective. Soft tissue laser procedures are indicated for restorations and crown preparation with subgingival margins, gingival recontouring, troughing in lieu of retraction cord, and the removal of small lesions
such as a fibroma. Non-initiated applications such as Laser Assisted Periodontal Therapy (LAPD) and treatment of herpetic type lesions to prevent a full breakout are also easily integrated into the clinical setting. By offering services to your patients who are often referred out of the office, there is value in adding a soft tissue laser to your practice.

FIG. 8
About the Author

Fred Peck, DDS, FAACD
Dr. Fred Peck is in private practice in Cincinnati, OH.
He is an accredited Fellow of the American Academy
of Cosmetic Dentistry, a Kois Center graduate, a
Fellow of the International College of Dentists and
a Dawson Academy graduate. His practice focuses on cosmetic and reconstructive dentistry. He has published numerous articles on cosmetic and restorative dentistry and
lectures throughout North America.
Discover More
This article was originally published in the Clinical Life™ magazine: Fall 2023 edition
Clinical Life™ magazine is a premier periodical publication by Clinical Research Dental Supplies & Services Inc. Discover compelling clinical cases from Canadian and US dental professionals, cutting-edge techniques, product insights, and continuing education events.
Subscribe to our emails to receive articles like this and be notified about our exclusive promotions.