
Just Take a Minute
The sheer volume of information on dental materials and techniques at our fingertips is staggering, but having the right information is vital to providing the best care possible.
Dental product marketing generally promotes ease, speed and cost savings as an advantage to change but we need to filter that information so that the techniques and products that we choose reflects our patients’ best interests.
Chair time is the most valuable commodity in the dental office, thus taking time to review treatment protocols makes a lot of sense. However, balance between clinical efficiency and continuing to provide dentistry of the highest quality is critical to any change you consider. Most of us get locked into a technique that we simply accept as “works best in my hands”. If we take a minute to consider the challenges that we experience in our day-to-day dentistry, many can be solved with just a small change in the technique or product we use.
The anterior composite restoration continues to improve in both its esthetic potential and efficiency of placement. Each step of this procedure should be considered, as current research and techniques show capacity for significant improvement; in adhesion, getting the most out of your composite, and the development of a more effective finishing and polishing technique. Just take a minute to break down your anterior composite technique into its component parts. Evaluate each step to determine if there are some changes that can be made to improve both your efficiency and clinical result.
Start by considering if your choice of phosphoric acid is the optimal strength and viscosity. Runnier H3PO4 gels tend to be more difficult to control during placement, leading to potential sensitivity. As well, many of us turned to self-etch adhesives due to postoperative sensitivity linked to the total-etch adhesive technique and “how wet is wet” dilemma. While there was far less sensitivity, I experienced some esthetic challenges. Occasionally, white lines appeared at the margin after polishing, and the formation of marginal staining was sometimes noted due to the inadequate pH of the self-etch adhesive. In hindsight, the bond strengths of the 4th and 5th generation or total-etch adhesives are considered the highest and most enduring, compared to the later generations. The simple addition of a glutaraldehyde-based desensitizer helps to solve the question of “how wet is wet”, as well as the post-operative sensitivity that is sometimes linked to the total-etch technique. Recent research into MMPs and their bond degrading activity makes it necessary to reconsider the choice of adhesive in its ability to inhibit their effect. The adhesive technique of choice should be easy to apply, universally compatible with all substrates and provide high, predictable bond strengths that are resistant to MMP degradation. Just take a minute and ask yourself if your adhesive choice satisfies these requirements.
The ability to match shade and opacity, place and thin the composite to a feather edge, establish contours without slumping and polish to, and retain, a high luster are all important to an esthetic restoration.
Anterior preparations have generally required bevelling to hide the margin and blend the restoration into the surrounding tooth. Despite this, it was always disappointing to go through a strict anterior composite regimen and still see the margin after polishing. Some composite systems today can provide the range of shades and opacities/ translucencies that enable the dentist to more easily blend the restoration into the tooth with less layers. I remember the frustration of having composite stick to my instrument, resulting in pull-back or lifting off of the tooth when trying to thin out the margin of the restoration or adapting it into a preparation. Some of today’s composites allow for easy placement of an infinitely thin margin without any pull-back. Coated instruments, available in many tip forms and thicknesses, allow improved placement, adapting, and sculpting of the composite. Would a change in your composite material and instrumentation improve your technique efficiency and composite restoration?
Finishing and polishing is one aspect of the technique whose importance is often overlooked. Many of us use discs for gross reduction, refining and final polishing. It is now possible to dispense with the finer grit discs and polishers of various shapes. Newer two-step, single shaped polishers produce an ultra high luster in less than a minute without degrading surface anatomy or diminishing the characterization of the restoration. Surface texture can be easily created by reducing the speed of a fine diamond and maintained with the right diamond polish. Take a minute to consider if your polishing regimen provides the efficiency as well as the flexibility to recreate form, texture, and luster of your anterior composites.
In order to desire an alteration in technique, it must be perceived that a change will better serve our patients. By just taking a minute to re-assess each step in your composite technique, perhaps you will discover that what you perceive as a challenge can be solved with just a little alteration to your technique. If not, you can remain confident that your approach is the best for you.


Dentistry and photography courtesy of Dr. Todd C. Snyder, DDS, FAACD. All rights reserved by Dentistry Today.
STEP #1: Mock up & Matrix
The traditional method of restoring existing Class IV composites, or replacing anterior tooth structure due to trauma, is to place and contour the composite by hand instrumentation.
If the length and lingual contour of the existing restoration is ideal, making a record of this preoperatively and using it as a template can greatly simplify the layering of dentin and enamel composite opacities and dramatically reduce the finishing time. In the case of trauma, simply mocking up the ideal lingual and incisal aspect using old or unwanted composite prior to making this lingual matrix will have the same effect. Fig. 1
Template® Ultra Quick MatrixMaterial from Clinician’s Choice is a silicone material designed to make highly detailed provisionals; however, its fast working and set times (30s and 30s), in addition to its accuracy, make it a perfect choice for this lingual matrix technique. Utilizing the Template lingual matrix technique dramatically reduces procedure time, provides the ideal lingual/embrasure contours, and leaves a pre-polished lingual surface.

FIG. 1
A composite mock-up is used for color assessment, establishing overall shape, and to fabricate a Template lingual matrix. Dentistry and photography courtesy of Dr. Todd C. Snyder, DDS, FAACD
Technique Tips
When mocking up a Class IV, only the lingual aspect and length of the restoration need to be ideal prior to taking the Template lingual matrix impression.
Cover the lingual surfaces of all six anterior teeth in sufficient thickness Template for matrix stability.
Limit the Template impression to the facial buccal line angle. This is to ensure that the proper length is captured with overlapping the Template onto the buccal surface. If this does occur, simply remove the excess Template with a sharp blade.
Load the first increment of composite into the Template lingual matrix and carry it to the tooth. Join the composite to the tooth once the Template lingual matrix is in place and cure.
STEP #2: Desensitization
Prevention of post-operative sensitivity is determined by the quality of the dentin/adhesive seal. Class I and II restorations are most prone to sensitivity due to the sheer size of the preparation as well as the number of adhesive walls involved. Ensuring your adhesive is properly applied and controlled so that all adhesive walls are sufficiently sealed is crucial. A properly applied adhesive obturates the dentin tubules which eliminates intra-tubular fluid pressure changes, preventing post-operative sensitivity. Utilizing a Glutaraldehyde-based desensitizer takes the guesswork out of dentin bonding by helping to obturate the dentin tubules before adhesive placement.
G5™ from Clinician’s Choice contains 5% Glutaraldehyde, HEMA, and water – the combination of which helps coagulate intra-tubular fluid proteins, resulting in a partial/initial dentin seal. Once G5 is applied, followed with MPa™ Max adhesive, together they create consistently high bond strengths and an ideal dentin seal to ensure the likelihood of postoperative pain is virtually eliminated. The use of G5 is not restricted to posterior restorations; it can be very effective in anterior restorations when dentin is exposed, as well as for desensitizing crown preps.
Technique Tips
Desensitizers are indicated when using a total-etch adhesive placement technique only (not with a self-etch technique).
After rinsing etch thoroughly, remove excess water from preparation with a brief blast of air, allowing for proper penetration of the desensitizer.
Always scrub the desensitizer for 10 seconds to ensure maximum penetration.
Remove excess/pooled desensitizer by damp blotting, leaving a moist surface before adhesive penetration. Never rinse after desensitizer placement.
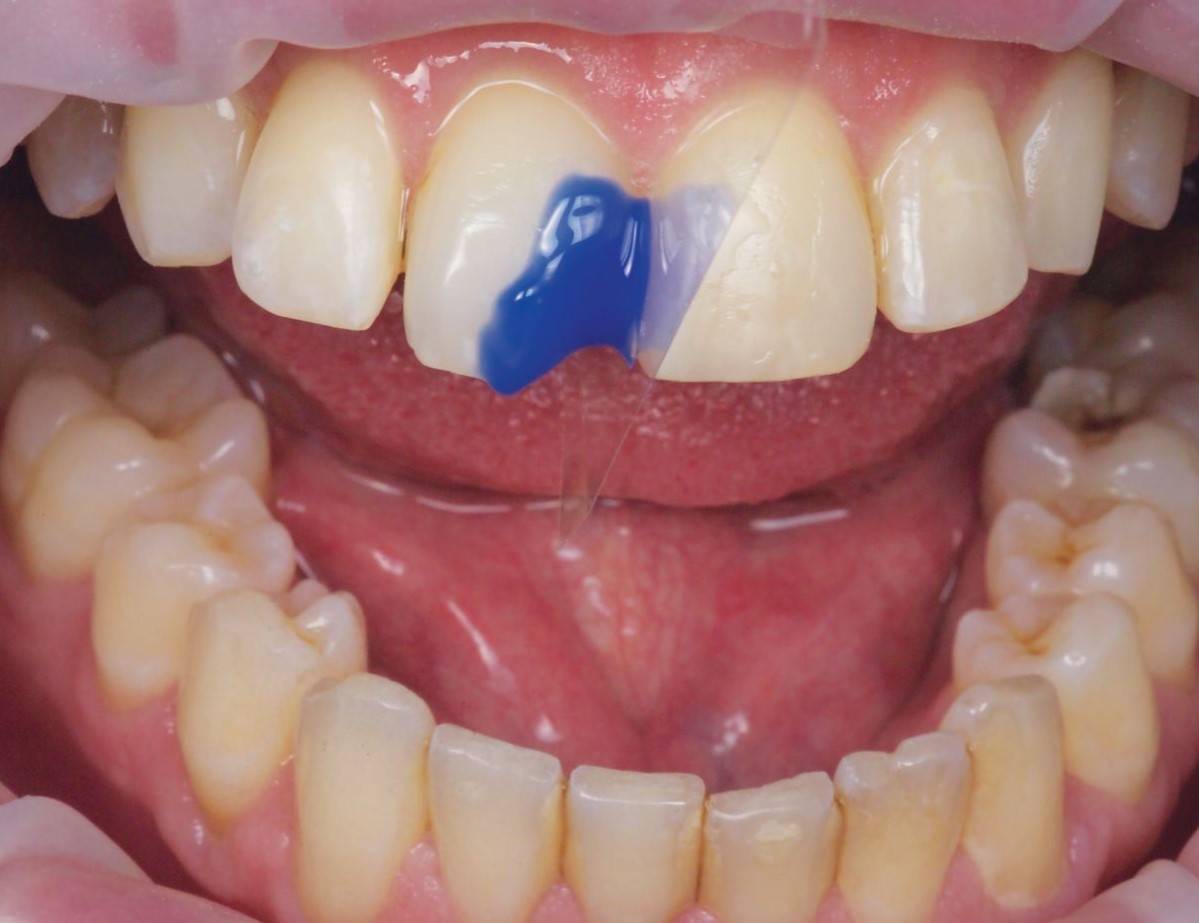
FIG. 2
Using a mylar strip for isolation, Max Etch is agitated on the enamel and dentin for 20 seconds, thoroughly rinsed and the surface air dried.
Dentistry and photography courtesy of Dr. Todd C. Snyder, DDS, FAACD
STEP #3: Etching
The bond to enamel is the most important bond and determines the longevity of your restoration as well as the integrity of the composite/enamel margin. The dentin bond is also key and determines the incidence of post-operative sensitivity your patients could experience. Your goal should be to achieve the highest bond strength as possible to both substrates. The total-etch technique provides the highest bond strength to enamel while demineralizing the dentin and removing the smear layer.
Max Etch from Clinician's Choice, a 35% viscous phosphoric acid included in the MPa™ Max Starter Kit, is easy to place, stays where you place it, and rinses easily; providing the best possible enamel conditioning. Fig. 2
Technique Tips
Etch for 20 seconds with H3PO4 (35%-40%) to ensure enamel margins are demineralized properly for maximum adhesive strength.
Agitate the etch on enamel margins to ensure fresh acid is in contact with the enamel margins.
Etch and bond beyond the bevel: Limiting where you etch restricts your ability to "feather edge" the composite, leading to visible margins and white lines after finishing.
Place etch on enamel margins for 10-15 seconds, then apply to dentin surface for and additional 5-10 seconds. Dentin requires less etching time as compared to enamel.
Bonding
The bond to enamel is the most important bond and determines the longevity of your restoration as well as the adhesive you choose must effectively and consistently seal the dentin tubules without being technique sensitive to apply.
MPa™ Max adhesive from Clinician’s Choice is designed to provide bond strength to both enamel and dentin of 45 MPa, one of the highest bond strengths available in dentistry. In addition, MPa Max is specifically designed for ease of application and to ensure a dentin seal is achieved with little technique sensitivity. MPa Max adhesive is slightly thicker than other adhesives, allowing for one coat application. This higher film thickness adhesive coats the adhesive walls, yet won’t over thin when air drying. In fact, MPa Max can be air thinned so just microns stay on the restorative walls to prevent post-operative sensitivity – especially when used in combination with G5 All- Purpose Desensitizer (also included in the MPa Max starter kit). With the addition of 0.2% Chlorhexidine, MPa Max is one of only a few adhesives that inhibit MMP breakdown of the adhesive bond. Fig. 3

FIG. 3
MPa Max is scrubbed onto the etched tooth surface for 10 seconds, air thinned, then light-cured for 10 seconds.
Dentistry and photography courtesy of Dr. Todd C. Snyder,
DDS, FAACD
Technique Tips
Air thin MPa Max with 1/2 air power for 5 seconds or until the MPa resin stops moving. Evaporate any remaining ethanol solvent with a gentle stream of air for an additional 10 seconds from one inch away from the preparation.
When using a self-cure composite or core material, remove the MPa Max O2 layer using alcohol. This will ensure a strong bond between MPa Max and the selfcure material.
Ensure each adhesive wall is coated; this often requires more than one dip into the mixing well.
STEP #4: Composite Placement
HIDING MARGINS
Technique and material selection are crucial to ensure invisible margins are created with anterior composite restorations such as Class III, IV and diastema closure techniques. Not all composites are created equal and few provide simplicity, strength and beautiful restorations. Challenges with handling and the inability to pre-shape anatomy without slumping or stickiness is common. This makes it necessary to use multiple opacity layers, tints, and opaquers which adds complication and inconsistent results. In addition, difficulty in shade matching or long polishing time requirements are frustrations that you don’t need to experience. Fig. 4, Fig. 5.
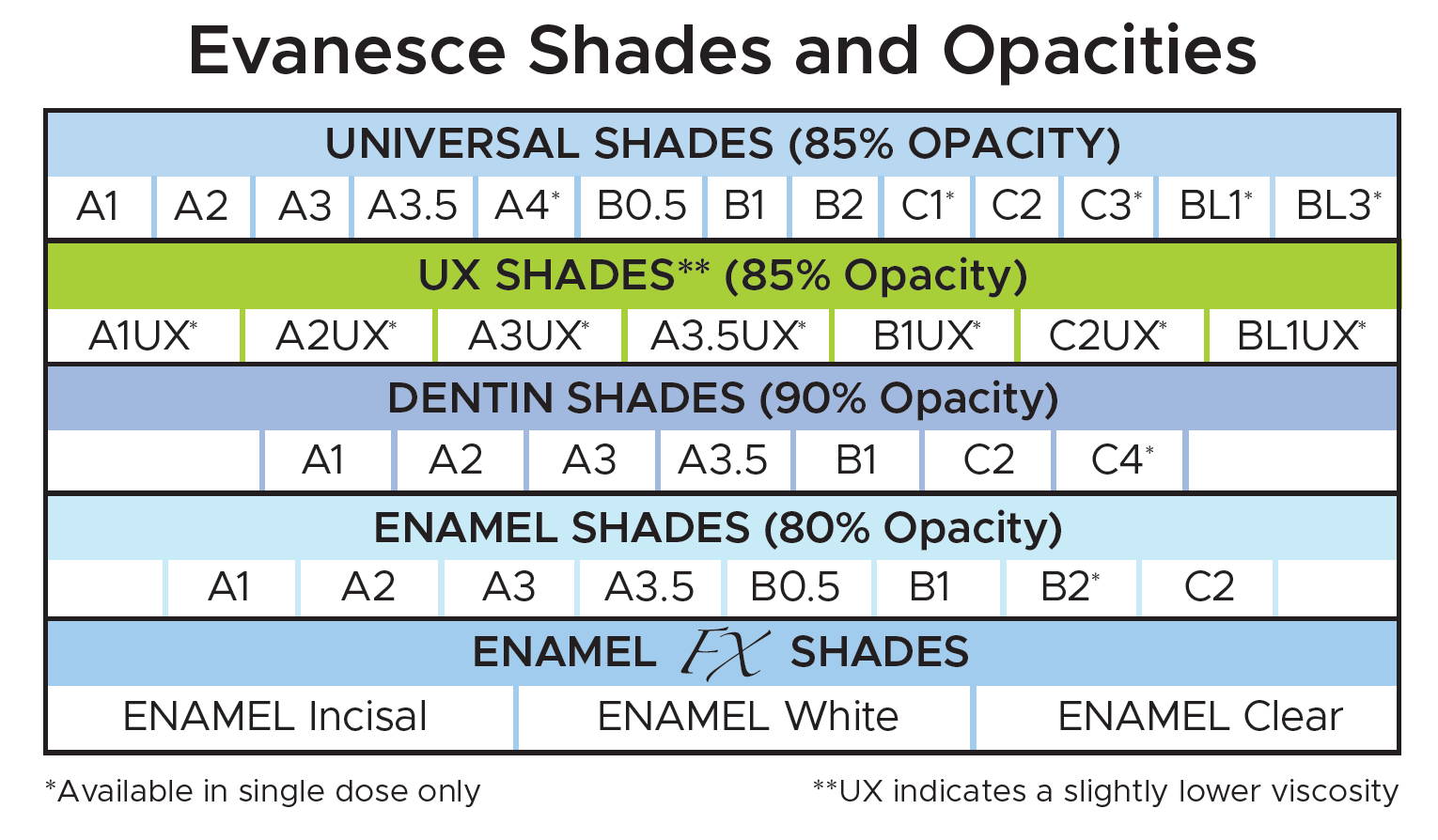
Evanesce™, from Clinician’s Choice, a nano-hybrid composite material is designed to give you simple, strong, and beautiful results for both anterior and posterior composite restorations.
SIMPLE
Evanesce™ users find that fewer opacity layers are required in most cases, compared to other composite materials. The unique rheological modifiers allow you to manipulate and shape Evanesce to create the most detailed anatomy without slumping. Designed with nano pigments and fillers to assist in blending with natural dentition, Evanesce restorations literally disappear. Ideal for both layered and single shade restorations, Evanesce comes in three opacities and 24 VITA shades, plus three Enamel non-VITA shades for characterization. For single shade cases, a second viscosity, Evanesce UX is available in 7 universal shades and features a slightly lower viscosity.
STRONG
82% filled by weight and with high compressive strength (340 MPa) and low wear (0.07 microns/200,000 cycles), Evanesce™ gives you confidence for both anterior and posterior restorations.
BEAUTIFUL
Evanesce™ matches the VITA Classic shade guide perfectly to provide efficient and consistent shade matching and has a unique ability to blend in with adjacent porcelain restorations. In less than one minute, you can polish Evanesce™ to a beautiful shine.
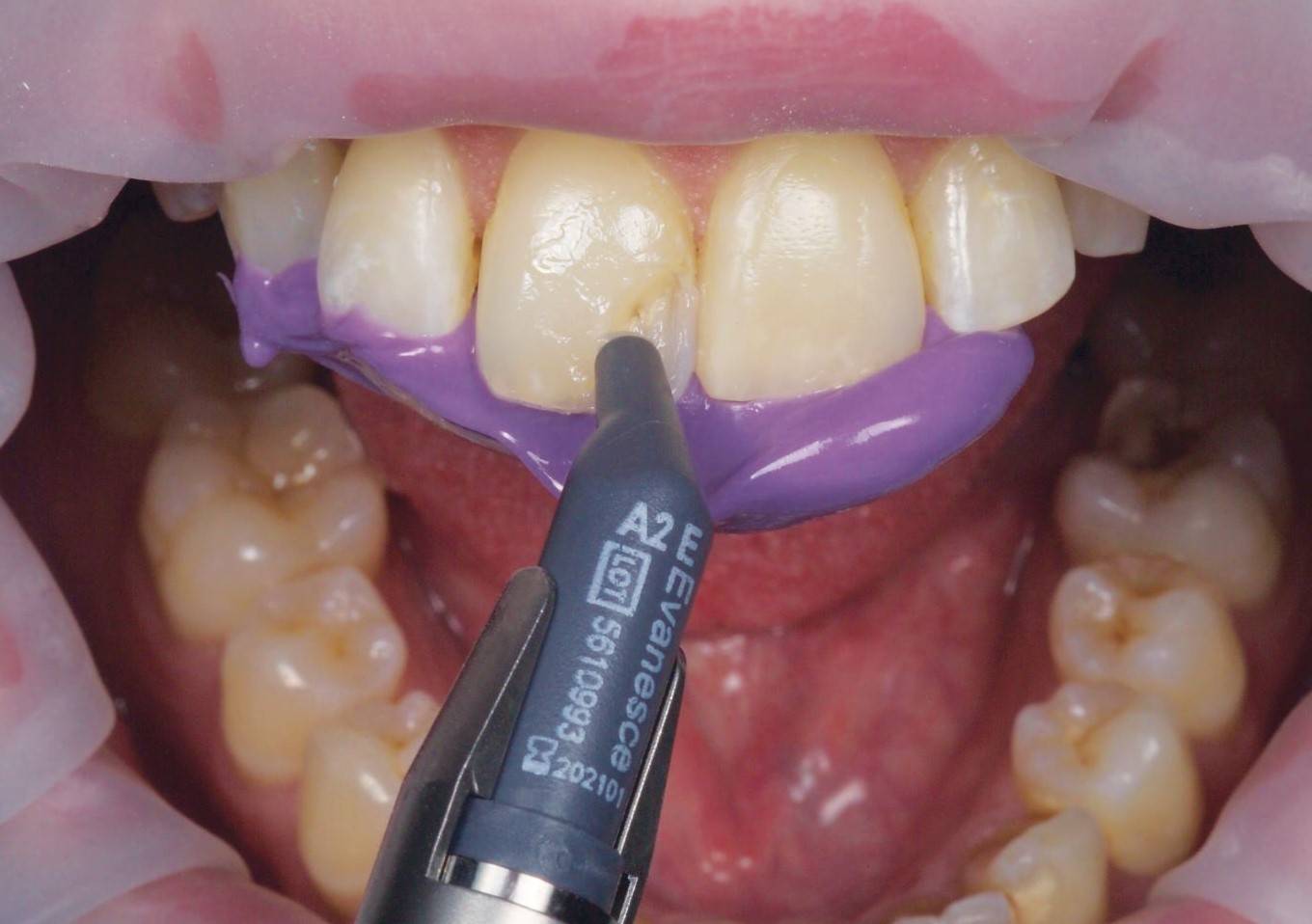
FIG. 4
With the Template lingual matrix in place, a thin layer of Evanesce A2 Enamel is applied, staying lingual to the facio-incisal line angle.
Dentistry and photography courtesy of Dr. Todd C. Snyder, DDS, FAACD
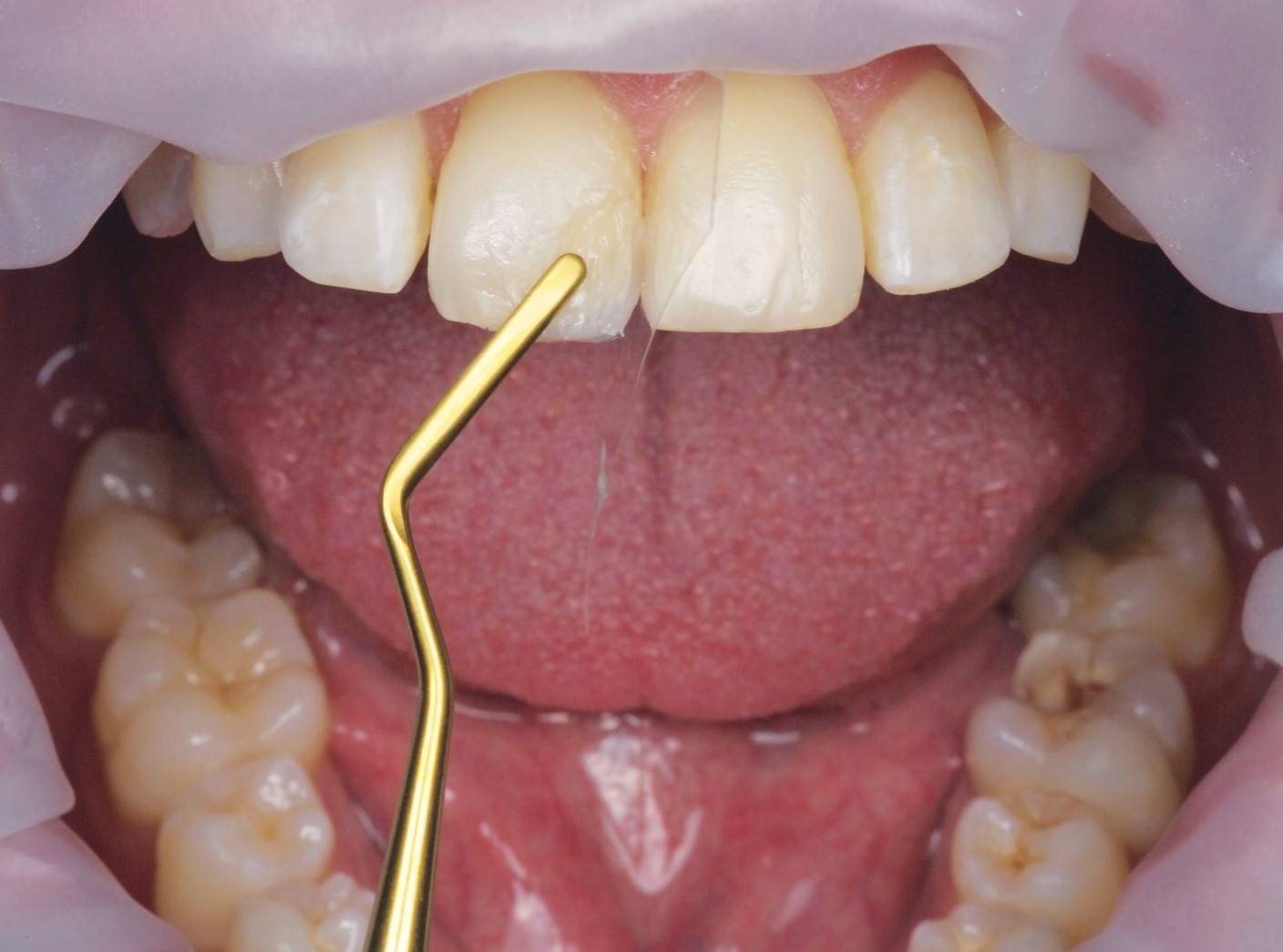
FIG. 5
Evanesce A2 Dentin is adapted to the enamel layer using an REJ #04, tapering the composite towards the incisal while varying its thickness to mimic a natural tooth.
Dentistry and photography courtesy of Dr. Todd C. Snyder, DDS, FAACD
Technique Tips
Always use a 2mm bevel: By extending the transition zone with a long bevel, you’ll take the first step in making margins invisible.
Understand your composite capabilities: Composite handling properties, opacity options, and filler content often determines the ease of which margins can be hidden.

STEP #5: Instrumentation
The choice of instrumentation for placing an anterior composite restoration can be beneficial in greatly reducing your placement and contouring time. Using instruments designed for ease of composite placement, shaping, thinning, and refining will allow you to better approximate the final anatomy of your restoration prior to light-curing. Stainless steel composite instruments are prone to scratching, resulting in frustrating pull-back of the composite during manipulation.
The Dr. Ronald Jordan (REJ) line-up of composite instruments from Clinician’s Choice provides an assortment of non-stick blades, thanks to their titanium nitrate precision designed tips. The REJ instrument blades are available in varying lengths, widths, and flexibilities so that you can place, shape, contour, and refine your composite prior to light-curing. Fig.6.
Technique Tips
Use the REJ #01 or REJ #02 with their broad, flat blades to place and compact the composite into the restoration. These instruments are used to start the spreading, thinning, and initial sculpting of your restoration.
The long, thin, flexible blades of the REJ #03 and REJ #04 are ideal to thin out the composite margins interproximally, where it is most difficult to finish after curing, as well as to establish an infinite margin facially. Use the length of the blades of these instruments to contour the line angles of the restoration.
Where tissue management is required, the REJ #03 can also be used for retraction cord placement.
STEP #6: Finishing
Final shaping, refining, and polishing of the anterior composite restoration is vital to its esthetics and longevity, yet the time allotted to this is often insufficient. While rotary instrumentation may be used for removal of excess composite and some refinement, the use of an aluminum oxide disc system can provide better control for the efficient gross reduction and refinement of the composite restoration as well as bring out the natural luster of the composite itself. Having the optimal flex and a choice of sizes will aid in gaining access to all aspects of the restoration without gouging the composite margin.
The Contours™ Finishing and Polishing Discs from Clinician’s Choice provide an easy to follow color/grit sequence along with ideal flexibility to allow efficient reduction, refinement and ultimately, a high luster polish. Contours Discs are available in the two most popular sizes of 3/8” and 1/2” diameters and effortlessly and securely pop onto a round mandrel. When used in sequence, the anterior composite restoration can be contoured, refined, and polished to a high luster in just a few minutes. Fig. 7a,7b.
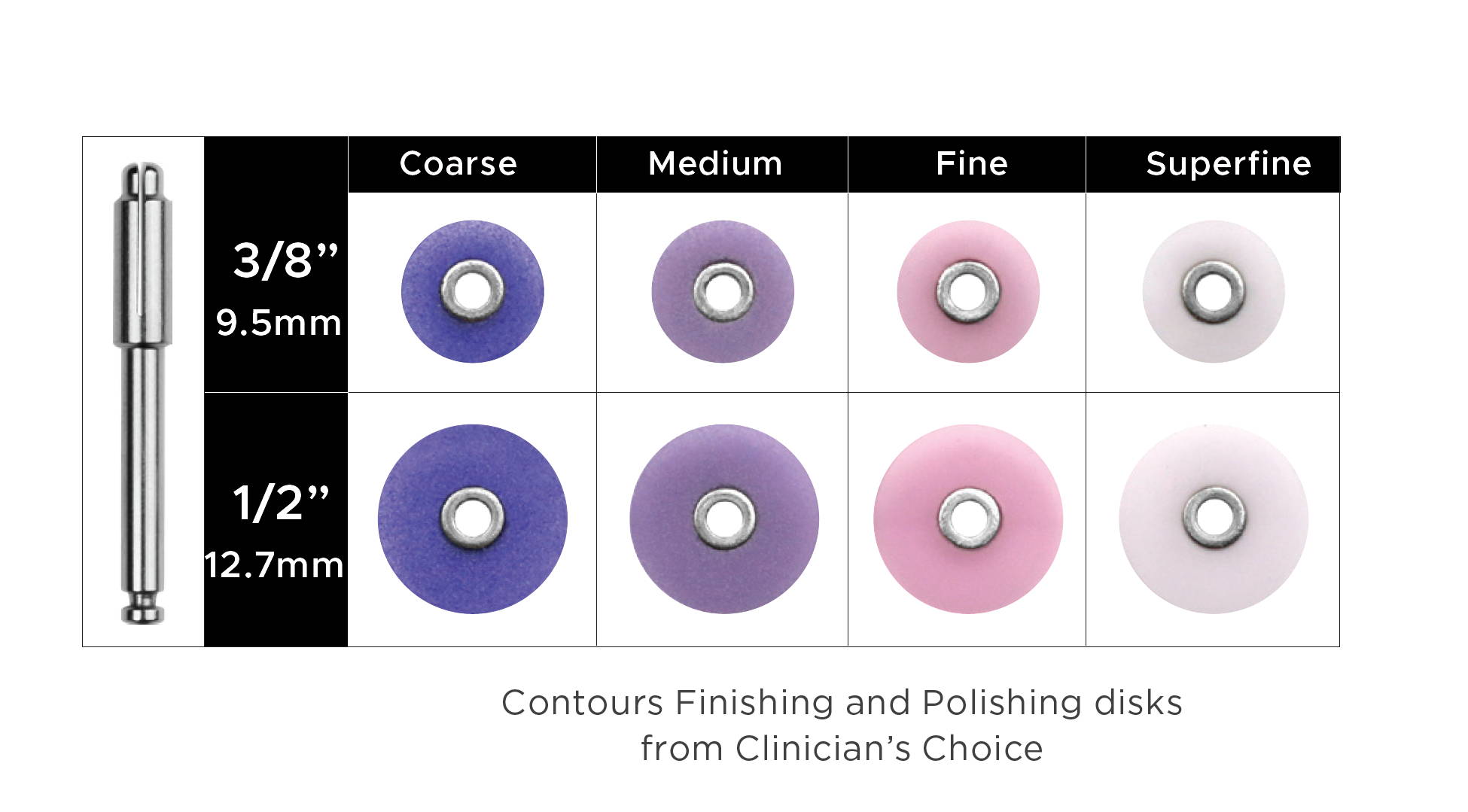
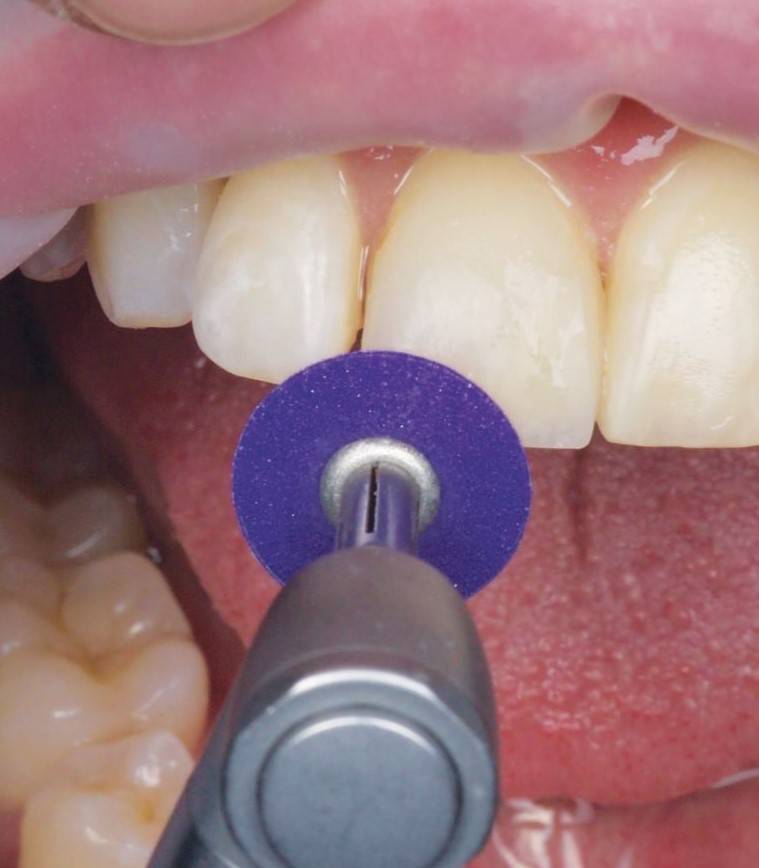
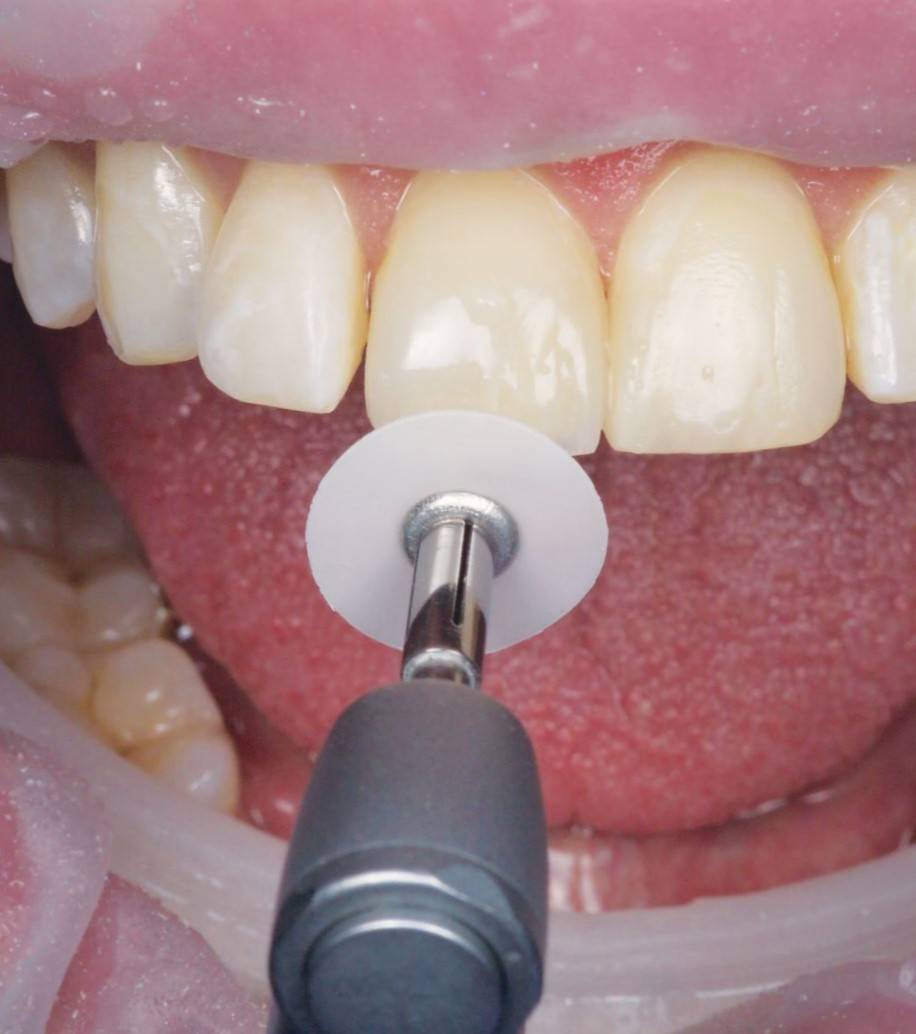
FIG. 7A, 7B
Contours Discs are used in sequence from coarse, medium, fine and superfine to reduce restoration thickness and length, refine contours and line angles, and produce a high luster polish.
Dentistry and photography courtesy of Dr. Todd C. Snyder, DDS, FAACD
Technique Tips
Using light pressure, keep the speed of the coarse and medium discs to approximately 10,000 RPM and the fine and superfine discs to approximately 30,000 RPM.
Use the smaller diameter (3/8”) discs for margins and areas near the papilla. Use the larger (1/2”) disc for larger surface area reduction, contouring and polishing.
Utilize the ideal flex of the Contours Disc by orienting it at 45° to the composite surface where possible. This will minimize the formation of planes or facets.
When surface texture is desired, use the coarse and/or medium discs at very low speed and light pressure, then follow with A.S.A.P.® All Surface Access Polishers.


FIG. 8A, 8B
Alternatively, once shape and contour are established and refined with coarse and medium Contours Discs, A.S.A.P. All Surface Access Polishers can be used to quickly and efficiently impart a high shine and surface luster.
Dentistry and photography courtesy of Dr. Todd C. Snyder, DDS, FAACD
STEP #7: Polishing
Once the finishing of your anterior restoration has been established, there is often very little time to achieve the ultimate polish. Polishing systems requiring multiple steps, shapes, and even polishing paste can be time consuming and frustrating.
Simplifying your polishing regimen to ensure that you have sufficient time to bring out the natural luster of the composite is achievable with the use of A.S.A.P.® All Surface Access Polishers from Clinician’s Choice. This two-step diamond polishing system utilizes one spiral shaped Pre-Polisher and one Final High Shine Polisher to create the highest luster in under a minute. The flexible, spiral-shaped polisher adapts to every surface of the restoration, eliminating the need to stock multiple shapes of polishers. Versatile A.S.A.P. Polishers are available in two sizes and are designed to be used on composites; however, they are also ideal for most ceramics, zirconia, lithium disilicate, and provisional materials. Fig. 8a, 8b.
Technique Tips
Use the larger diameter (14mm) A.S.A.P. Polishers for most anterior composite restorations. Use the smaller (10mm) A.S.A.P. Polishers for posterior composites and pedodontic restorations.
Do not use the A.S.A.P. Polishers in reverse as this will cause excessive wear and possible breakage of the polisher.
The purple Pre-Polisher should be used for 20 seconds prior to proceeding to the peach-colored Final High Shine Polisher. A minimum of 10 seconds is all that is required to achieve the highest luster.
A.S.A.P. Polishers may be substituted for the Fine and Superfine Polishing Discs in the Contours Finishing and Polishing Disc system.
About the Authors

Douglas Harvey
BSC, DDS
Dr. Harvey has been a long-standing member of the International Dental Study Club, and has served in organized dentistry at the local and provincial levels in Canada.
Dentistry and
photography courtesy of
Dr. Todd C. Snyder,
DDS, FAACD
Dr. Snyder is the 77th Accredited Fellow of the American Academy of Cosmetic Dentistry and is a Fellow of the International Academy of Dental Facial Esthetics. He is also a member of the American Society for Dental Aesthetics and a Diplomat of the American Board of Aesthetic Dentistry.
Discover More
This article was originally published in the Clinical Life™ magazine: Fall 2019 edition
Clinical Life™ magazine is a premier periodical publication by Clinical Research Dental Supplies & Services Inc. Discover compelling clinical cases from Canadian and US dental professionals, cutting-edge techniques, product insights, and continuing education events.













