Cementation Technique for Monolithic Zirconia Crowns
The last decade which is now behind us provided the largest increase in zirconia usage for monolithic restoratives. No bigger change has occurred within dentistry as the move to all ceramic restorations. Non-metal based restoratives are at an all time high. The reasons for this switch are many: ease of use, easier lab fabrication, strength, metal-free, traditional cementation, esthetics, cost, value to the dentist and the patient. The short term results in vivo have been largely very successful (Fig. 1).
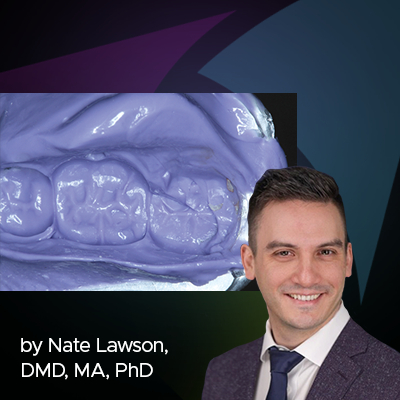
The overall strength of zirconia allows it to be traditionally cemented when a full understanding of the best conditions are available. Typically a zirconia crown could be traditionally cemented when you have at least 2 mm of circumferential tooth structure supra-gingival with adequate 6 degrees of taper, and adequate retention and resistance form (Fig. 2, 3). If these criteria for retention are not available to the clinician, a more suitable choice would be a resin cement with either all in one properties (Unicem 2) or the addition of a separate self etching primer for more adhesive strength (RelyX Ulitmate 3M).
RMGI cements have been out for many years. They have a long and proven track record for traditional cementation of All Gold restorations, PFM’s, and now All Zirconia, Monolithic crowns as well. 3M/ESPE RelyX line of RMGI’s have had over 20 years of excellent long term results. The material of choice these days are auto mixed in a dual barrel chamber, that when dispensed, it is also light curable, “freezing” the material expressed around the crown margin, while the material is auto curing.
The most efficient and best practice for cementation of monolithic zirconia crowns:
1. Try in the restorations, adjust the contacts, and if needed occlusion, polish with the appropriate zirconia polishers like A.S.A.P. All Surface Access Polishers from Clinician’s Choice.
2. Then, either microetch the internal surface with 30 micron alumina oxide or clean the internal surface with a surface treatment of Ivoclean (IvoclarVivadent) or Zirclean (Bisco) (Fig. 4).
3. Rinse and dry, then coat the internal surface with and MDP containing zirconia primer like Z-Prime (Bisco) (Fig. 5), that supports chemical adhesion of cements to the zirconia restorations. In my practice, I like to separately apply the zirconia primer.
4. Then the material is expressed into the individual crowns and seated.
5. A quick 5-second cure with the LED curing light to help set the material that is expressed on the crown margins (Fig. 6), then let set for 3 minutes to auto cure.
6. Removal of the excess cement is quite easy with RelyX Luting Plus while proper flossing and rinsing to remove and remnants of cements is recommended. Utilizing the same sequence of the steps ensures long lasting restorations that provide years of use with little to no post operative sensitivity for the patient (Fig. 7, 8).
About the Author
Robert Ritter, DMD
Dr. Ritter has a practice that focuses on adhesive esthetic dentistry. He promotes esthetic dentistry as part of his main stream dental care. He was raised in Palm Beach County and now resides in Palm Beach Gardens.
Discover More
This article was originally published in the Clinical Life™ magazine: Winter 2020 edition
Clinical Life™ magazine is a premier periodical publication by Clinical Research Dental Supplies & Services Inc. Discover compelling clinical cases from Canadian and US dental professionals, cutting-edge techniques, product insights, and continuing education events.
Access previous publications, request print editions, or subscribe to our Newsletter now. Join our thriving dental professional community and take your practice to new heights!
Subscribe to our emails to receive articles like this and be notified about our exclusive promotions.