An Ivoclar OptraGate® was initially placed, and the teeth were dried and treated with Bioclear Disclosing Solution for 10 seconds before rinsing. This exposes the protein pellicle and any biofilm. Teeth 13 to 23 were treated with a slurry of water and Bioclear Blasting Powder (aluminum tri hydroxide particles) using the Bioclear Blaster, to remove any surface contaminants.
Bioclear TrueContact Saws were then inserted at each point of contact to ensure patency for the upcoming matrix seating. Bioclear Black Triangle Matrices are made of mylar and have a 75 μm thickness. The more matrices seated in a row, the tighter the insertion gets. It is important to restore one tooth at a time and avoid multiple teeth set-up. The more matrices inserted at once, the more aggressive interproximal stripping must get. It is a compound effect of the 75 μm-thickness of each matrix. The clinician must ensure to retain proximal contacts when possible.
Once all necessary arch-form adjustments and incisal cutbacks were performed, the rubber dam was placed. Tooth number 11 was established as the guiding tooth from which to build the rest of the segment. Therefore, it is injection moulded first and cut back to 80% of its final shape.
37% phosphoric acid is used to etch the entire surface of tooth 11 for 15 seconds, prior to rinsing. All of the excess water is removed, and 3M Scotchbond™ Universal Plus Adhesive is used to scrub any freshly cut or exposed dentin for 20 seconds. The adhesive is air-thinned to evaporate any solvents. After the adhesive is cured for 10 seconds, it is again used generously, but this time as a surfactant (wetting agent) in order to lubricate the intaglio of the aquarium. No curing is required at this step.
Heated 3M Filtek™ Supreme Flowable restorative is slowly injected inside the matrices bracing the tooth. The tip of the canula is inserted from the facial and aimed interproximally toward the palatal. A slow and measured injection method is necessary to prevent the entrapment of air bubbles.
Following the placement of the flowable resin, warmed 3M™ Filtek™ Supreme Ultra Body Composite paste is now injected into the system. It is a density game: the surfactant is displaced by the more viscous flowable resin, which in turn gets pushed out of the way by the dense composite paste. All in all, the final restoration is roughly a 90% monolithic, densely packed composite paste. As shown in Fig. 7, there is an overabundance of material extending beyond the incisal edge of tooth 22. As
the flowable resin is displaced incisally by the denser composite paste, it may trap air bubbles. Failing to add a sufficient amount of paste during the injection-molding process may result in holes or voids at the incisal border during cut-back.
The over-molded tooth is polymerized, 10 sec per plane—incisal, mid, and gingival planes, both facially and palatally. Depth of cure must be ensured with intentional curing.
After disassembly of the aquarium, the tooth is roughly cut-back to 80% of its final shape using a Komet (Clinical Research Dental) coarse diamond flame-shaped bur and a 3M Sof-Lex Coarse disc. It is strongly recommended to re-cure the composite after cutback because 3M Filtek Supreme Ultra Body has a depth of cure of 2 mm. This will ensure to neutralize all yellow, light-sensitive camphorquinones and reach the intended shade for the restorative material.
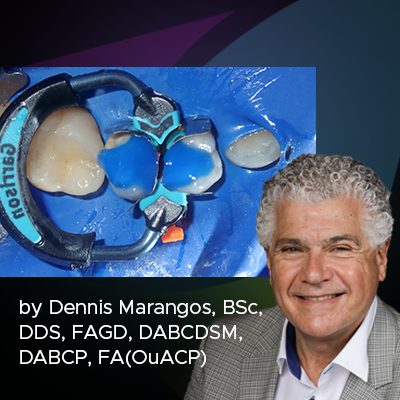
Onto restoring tooth 21. Bioclear blue and green large black triangle matrices brace the tooth on the mesial and distal. This forms the Bioclear aquarium into which the injection moulding takes place. In addition, matrices brace the adjacent teeth in order to preserve their upcoming and final shapes. We call these shield matrices (Fig 6).